“I am tired of hearing the government talk about ‘post-Ebola’. It is already too late, things are happening now and we can’t wait for things to improve to change. It is time for action”.
Dr Bintu Mansaray (Connaught Hospital, Freetown) to ARI, June 2015
While Ebola has killed 3,933 Sierra Leoneans, “huge numbers of people are dying from avoidable causes” says Dr James Elston, author of a recent report by Médicos do Mundo.
The report sheds light on the dire impact Ebola has had on tackling preventable diseases. It cites drastic drops in attendance at health facilities, poor availability of supplies and growing mistrust between the health care system and the communities it is supposed to serve as the causes of rising death rates.
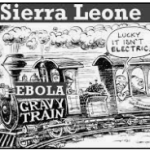
Belatedly, the question of post-Ebola reconstruction of the health system is now being debated. Despite the substantial investments made by international donors such as the UK’s Department for International Development (DFID) between 2002 and 2014, and the vast quantities of emergency funding received during the Ebola epidemic, the health system in Sierra Leone remains wholly unfit for purpose.
The majority of Ebola treatment centres are expected to be dismantled once ‘zero cases’ has been achieved. This is because of stigma, their lack of connection to basic infrastructure such as roads, water and electricity and, because there are simply not enough staff to operate them. This underscores the importance of creating a sustainable, ‘context specific’ health system in Sierra Leone.
What stands in the way of this being achieved?
There are arguably three main obstacles:
- A lack of trust in government, an issue that extends beyond the provision of basic health services. In particular, the failure to deliver on the promises of the 2010 Free Healthcare for All Initiative, which has been undermined by petty corruption. The absence of trust was discernible right at the outset of the epidemic, for example when residents of Kailahun district proved distinctly unreceptive to advice issued by the government and its international partners about preventative measures.
- Recruiting and retaining health care workers. Salaries and incentives need to be offered that enable staff to advance their skills and improve retention. About half of the medical staff trained in Sierra Leone leave for Ghana, the UK and elsewhere.
- Poor basic infrastructure. Poor access to water was a major hindrance at Ebola treatment centres. Electricity supply is sporadic, at best, and limited in reach. Generators often lie idle as hospitals and other health facilities have no money for fuel. Ambulances capable of navigating roads in rural communities are in short supply. The centralised dispensation of drugs is not done with sufficient district level input, meaning that local health facilities often lack one or two key drugs that would improve treatment of leading afflictions in rural communities.
A strategy built on local expertise
Local health experts must be the bedrock for improvement of health care. Here are some recently-voices opinions from three of them:
- Dr Bintu Mansaray told ARI that conditions for health care workers must be improved. “We need the supplies, training and incentives; currently we don’t even have risk allowances or health insurance”. At the moment, patients see hospitals as a “place you go to die, not to be cured”.
- Dr Haja Wurie (College of Medicine and Allied Health Sciences) stresses the need for services to be accessible to all. “The government should find a way to incorporate traditional healers in this process, while emphasising the primacy of health facilities”.
- Felix Conteh, who worked with the World Bank on decentralisation in the health sector, told ARI that a long-term approach is needed. Crucial to its success will be “ensuring that conducive conditions are created for health workers, as well as establishing mutual accountability mechanisms between them and the government, whether at the centre or the local level”.
Ebola did not decimate the infrastructure of a functioning, adequate health system – there was no such thing. However, it ravaged skilled human resources. The government needs to acknowledge the contribution of health professionals who have died and ensure that employment conditions and facilities in future will enable their successors to build a functional health system. This would be a crucial first step on a long road to rebuilding trust in the government’s seriousness about providing basic health care for the people.
Jamie Hitchen is a Policy Researcher at the Africa Research Institute.