As Director of the Situation Room at Sierra Leone’s National Ebola Response Centre (NERC), OB Sisay played an important role in countering the outbreak of Ebola that afflicted Liberia, Guinea and Sierra Leone in 2014 and 2015.
As Director of the Situation Room at Sierra Leone’s National Ebola Response Centre (NERC), OB Sisay played an important role in countering the outbreak of Ebola that afflicted Liberia, Guinea and Sierra Leone in 2014 and 2015.
President Ernest Bai Koroma established NERC on 18 October 2014, in an attempt to bring greater coherence to the response to the Ebola crisis. The centre progressively put in place systems and measures to support those striving to stem the rate of infection and end the outbreak.
In this interview with Jamie Hitchen, policy researcher at Africa Research Institute, Sisay reflects on Sierra Leone’s handling of the emergency. At the outset, citizens’ lack of trust in the government and poor coordination of international assistance severely hindered the efficacy of the response. But lessons were quickly learned.
Sisay stresses the importance of local ownership and decentralising decision-making; and hopes that structures and approaches used to tackle Ebola will be replicated more widely in Sierra Leone to good effect.
INTRODUCTION
By Jamie Hitchen
The Ebola virus arrived in Sierra Leone in 2014 through the porous borders with neighbouring Guinea. The first official case was recorded on 24 May in Kailahun district, in the south-east of the country. By July, it had reached the capital city Freetown. The following month, and with infections increasing significantly by the week in Guinea, Liberia and Sierra Leone, the World Health Organization (WHO) declared the outbreak an international health emergency. In the fifteen months before Sierra Leone was pronounced Ebola-free, 14,124 cases were recorded (suspected, probable and confirmed), with a mortality rate of 28%.1
Initial responsibility for coordinating the response in Sierra Leone rested with the Ministry of Health and Sanitation. Widespread criticism of its ability and capacity led to the sacking of the health minister, Miatta Kargbo, in August 2014. In October, as the number of cases threatened to spiral out of control, President Ernest Bai Koroma announced the creation of the National Ebola Response Centre (NERC). Funded by the UK’s Department for International Development (DFID), with additional support from the US-based Centers for Disease Control and Prevention (CDC) and the United Nations Missions for Ebola Emergency Response (UNMEER), NERC was tasked with collecting and analysing real-time data to inform decision-making.2
NERC’s role in getting a grip on the situation was significant. It enabled the gradual emergence of a degree of trust in local communities, the decentralisation of aspects of the response and the affirmation of national ownership of a crisis that, towards the end of 2014, was taking on a global dimension. International assistance, and human and financial resources, played a vital part in defeating Ebola, but their impact was greatest when deployed in collaboration with local agencies and communities. Local health care workers were the unsung heroes. Despite huge personal risks, they persisted in attending to their fellow citizens. Eleven of Sierra Leone’s 123 medical doctors died. Across the region more than 500 health care workers perished.
Sierra Leoneans rejoiced on 7 November 2015 when the country was declared free of the virus. However, the crisis exacerbated many pre-existing problems: the inability to provide functional and decent public services; a lack of accountability and trust between state and citizens; and poor coordination of government. These remain unaddressed. Learning how an institution like NERC was able to excel is important if Sierra Leone is to build more responsive, transparent and effective systems for delivering public services.
February 2018
ON LOCAL OWNERSHIP
You have spoken frequently about the importance of local ownership of the response. Why was this so important? How did you go about ensuring Sierra Leoneans were to the fore?
Until the creation of NERC, the Ebola response suffered from a lack of national ownership and coordination. In the first few months, it might be the case that in one district there would be six different outfits, predominantly international organisations, working on social mobilisation messaging and in the neighbouring district there would be none. In addition, two-thirds of those organisations would be using messages that had not been approved by government. These messages, which highlighted the deadly nature of the disease and the absence of a cure, intended to promote protective behaviours, but had the opposite effect. With the understanding that death was inevitable, many chose to eschew hospitals and receive care at home from friends and family, who then themselves were infected. The whole social messaging exercise was happening without clear direction from government about what the messages should be, who should deliver them, how – and whether – it was altering public attitudes and behaviour. The lack of strategic national leadership was glaring.
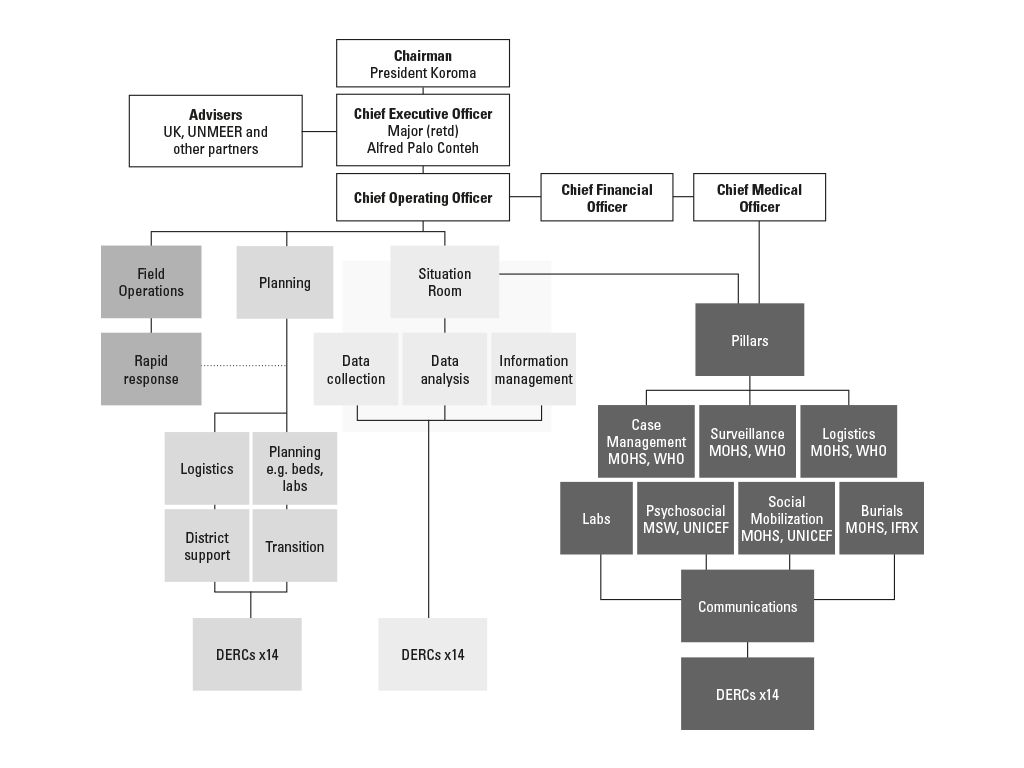
After the creation of NERC (see Figure 1), a daily morning briefing was instituted, but problems persisted. Everybody involved in the response, from civil society to NGOs to journalists, attended. Meetings went on for several hours while people pontificated and held forth with speeches. This was supposed to be an incident management centre that provided brief updates on the current situation. NERC was not an expert Ebola-fighting organisation. Its function was to provide command, control and direction so that the Ebola fighters, the experts, could do their job most effectively. These elongated meetings were not helping it do this. But there was a more fundamental problem.
At that time, the Operation Gritrock people – the British-led military taskforce sent to assist the Ebola response, the UK’s DFID, and the local British High Commission officials – convened their own meetings, where they got their own data and reports from the field and decided what they would do next. As the government’s primary partner, both during the crisis and in development assistance, the UK view had a great deal of clout, but it was not being conveyed in a very transparent way. There was also a regular donor partners’ meeting where a common position was discussed. In fact, the only group that were not having separate meetings to discuss their position were Sierra Leoneans. Following internal discussions at NERC, I took the advice of my team to Maj. (Rtd) Paolo Conteh, the chief executive officer of NERC, and suggested replacing the daily morning briefings with twice-weekly Command Group meetings and follow-up Coordination Group meetings.
By owning the management of the response, Sierra Leoneans demonstrated their commitment to tackling Ebola; and by allowing them to do so, the donors demonstrated confidence in the ability of nationals to own it
The Command Group meeting would comprise Sierra Leoneans only.3 The Coordination Group would comprise members of the Command Group plus international partners.4 Purely Sierra Leonean matters would be discussed in the Command Group meetings and the following day, once a position had been agreed, the donor partners would be involved. Everyone was allowed to offer their opinion, but the final decision was to be taken by Maj. Conteh.
In the beginning, we got a lot of pushback from international partners who felt that we were locking them out of the decision-making process. This was not the intention and quickly this became obvious, but not before we had to make a few points about sovereignty and the importance of Sierra Leone having its ducks in a row before engaging with others. In fact, this system gave partners a formal mechanism to influence decision-making, whereas previously they had to rely on the strength of their bilateral relationships. Even recalcitrant NGOs gradually came round to seeing the benefits of having a central body they could direct questions to, raise concerns with and demand answers from.
The approach created a more inclusive environment, which allowed all those involved to have their say on the direction of the response; and it placed the ultimate decision-making in the hands of national, not international, leaders. The collegiate approach adopted – one that allowed everyone to have their input, share their concerns and outline their capabilities – gradually transformed the way the response was discussed. From “the British government will do this” and “WHO will do this”, it became “NERC will do this”. This singular voice was very important. By owning the management of the response, Sierra Leoneans demonstrated their commitment to tackling Ebola; and by allowing them to do so, the donors demonstrated confidence in the ability of nationals to own it.
ON BUILDING TRUST
A lack of trust between citizens and the government in Sierra Leone, combined with unhelpful messaging about Ebola at the beginning of the outbreak, made it very difficult to contain the virus. How did NERC attempt to build trust with communities across Sierra Leone?
In November 2014, six months after the first case of Ebola in the country, there was still no Sierra Leonean organisation undertaking comprehensive, nationwide data collection about the spread of the virus. Decision-making at government level was reliant on data provided by external actors. UNMEER and WHO, for example, were reluctant to share what they had with the government and each other. This meant that on any given day the Ministry of Health and Sanitation, CDC and WHO would have different figures for the number of Ebola cases that had been recorded.
To address the coverage, control and quality of information, a working group was established by NERC in November 2014, comprising all domestic and international stakeholders involved in the response and collecting data. In the initial meetings, it was agreed to reduce the number of key indicators that we needed to collect data on from 150 to 40. These included everything from the number of people dead to the number of social mobilisation messages disseminated. We agreed to have core indicators around infections, deaths and so forth, and who was to collect what. This was driven by a belief that “the only chain that matters is the chain of transmission”, so any data collected had to be shared with others on the ground before being disseminated to Geneva, London or anywhere else these agencies had their headquarters. Of course, we didn’t achieve this in the fullest sense, but by harmonising collection we managed to establish a “ground truth” on data – everyone was working on the same set of numbers collected by different organisations doing different things. It was important in that it allowed NERC to take evidence-based decisions, using figures that all stakeholders agreed upon.
Establishing the ground truth gave people confidence that reported Ebola case numbers in specific locations were correct. When questions were brought to our attention about a possible mis-diagnosis, we made it a priority to investigate. If it was found that an incorrect blood sample had been used, we would ask the head of the Ministry of Health’s laboratories – to whom all labs in the country, local and foreign, reported – to explain to the public on the radio, TV and in town hall meetings where necessary, that it was a wrong diagnosis and why the error had happened. If a medical explanation was needed, a health professional was asked to explain – in layman’s language – the reasoning for the discrepancy. Our approach was designed to be transparent, honest and not condescending.
NERC tried to overcome this inherent distrust of the centre by committing to transparency and opening itself up to external scrutiny
For many Sierra Leoneans, mistrust of the government is driven by their own experiences and interactions with the state, which often leave them less than satisfied. NERC tried to overcome this inherent distrust of the centre by committing to transparency and opening itself up to external scrutiny. We held a weekly press conference, created a website where all the analysis of the Situation Room briefings and data were published, and provided a room for the press within the NERC campus, with internet and printing facilities. We even started putting our quarterly financial reports online. This allowed people to see who cheques were being issued to, for what reason, and the amounts. We were able to do this by working closely with a team from the Office of the Auditor General, which carried out a real-time audit of our financial operations.5
Owning up to your mistakes, being open about the problems you face, and trying to explain how you intend to fix them is important for building trust. This is what NERC tried to do. Except for the initial phase of the response, when people did not trust government at all, we were able to bring the population along with us. Sierra Leone did not experience demonstrations against the government, like in Liberia, or fatal attacks on health care workers, as happened in Guinea.
ON THE INTERNATIONAL RESPONSE
What would you say to international donors and NGOs that are looking to learn lessons from their response to Ebola in Sierra Leone?
The slow nature of the international response to Ebola has been well documented. When it was underway, a large majority of those working on the ground demonstrated extraordinary commitment and dedication, alongside Sierra Leoneans. However, there was still a lot of “disaster tourism” going on. International NGOs were bringing in people with qualifications that bore no relation to the terms of reference you see when you try and apply for jobs on their websites. These individuals were given astronomical salaries for a six-week period and then left, often without any proper handover to their replacement. The new arrival would then put their hand up in a meeting and be like, “I am from Geneva, I have all of the answers.” They would make you waste an hour of a meeting by bringing up things that had been discussed, examined and dismissed four months ago. I had a problem with that.
I also had a problem with the way donors handled funds that had been committed to the response. They did not behave in a way that suggested the funds were for the countries affected by Ebola. It was as if it was their own largesse, which we had to ask them politely for. In that, there was an implicit questioning of Sierra Leoneans honesty, ability and knowledge, which I found condescending.
The £43m treatment centre built at Kerry Town with British funding was emblematic of some of these problems.6 The idea was that the 100-bed facility would provide confidence to other countries to send their health care workers to support overwhelmed Sierra Leonean and international staff. Incredibly, at the start they considered building a facility that would not accept Sierra Leonean patients. Fortunately, they saw sense on that, but Kerry Town was just an expensive gesture that has done nothing to address long-term, systemic problems in Sierra Leone’s health system. If you go and visit it now, there is nothing but a few abandoned structures, and yet our hospitals and medical facilities remain underequipped to provide basic levels of care. At the same time, the Republic of Sierra Leone Armed Forces converted facilities such as the 34 Military Hospital, in Freetown, into effective treatment centres, at greater speed and a fraction of the cost. In February 2015, less than three months after it opened, over 800 Ebola patients had been treated there.7
As both a taxpaying British citizen and a Sierra Leonean, I would really like to understand the reasoning and decision-making behind spending £43 million on a project that appears to have so few long-term benefits. It’s a sum equivalent to our entire government budget for health in 2017.8 The money could, and should, have done so much for Sierra Leone’s health sector.
ON DECENTRALISING CONTROL
You have been quoted as saying “the fight against Ebola was not about building hospitals, but about changing attitudes. The importance of culture, local communities and traditional authorities in responding to Ebola was overlooked for much of the response”. How did NERC seek to adapt to this reality?
At the start, the lock, stock message was that if you had Ebola you were going to die: there was no cure. This drove people away from treatment facilities and into the hands of traditional healers. Even though they had been banned from practising, this was the reality. So we adapted our strategy to bring them on board. Educating traditional healers about the sort of symptoms a patient who has Ebola might show, and encouraging them to share that information with medical personnel and NERC, meant that they became an effective early warning system. Instead of trying to coerce the public, we sought to use these pre-existing local structures to both educate and inform at chiefdom level. To be able to change people’s behaviour, you need to speak to them in a language they understand and see things from their worldview. NERC’s leadership was made up of people who understood these cultural nuances. It was about shifting the onus.
Instead of saying the government is coming to fix the problem for you, we wanted local leaders to resolve the problem with our support. It was not lost on us that the districts that were able to contain Ebola first, places like Pujehun and Kailahun, had been able to do so before NERC was formed. They succeeded by using social structures and networks that were well established in the local community. We very quickly realised that it would be more effective to hand power to the people; we had to decentralise the way NERC operated. In many parts of the country, government only works by the grace and support of traditional powers.
In late 2014, District Ebola Response Centres (DERCs) headed by a coordinator and directly answerable to NERC were created. These were the district-level equivalent of NERC, but designed to be more adaptable to the local context. Up until that point, the entire response was being coordinated from Freetown when the majority of cases were in the eastern districts of Kenema and Kailahun. That was a mistake. A person on the ground in Kenema had a much better sense of how to respond to the outbreak and the DERC enabled them to get on and do it.
It was not lost on us that the districts that were able to contain Ebola first, places like Pujehun and Kailahun, had been able to do so before NERC was formed
The balance we sought was to find a way to decentralise responsibility and power, whilst ensuring accountability was retained – “accountability” in the sense that, if Ebola was getting out of control in a district, NERC could liaise with one person to give them an account of what was going on, what was needed and the support they required. It was not about accountability for the purpose of apportioning blame. Handing power away from the centre made a big difference.
ON LEARNING FOR THE FUTURE
What are some of the key lessons learned by NERC that you would like to see the government take on board and implement in the future? Has the government been receptive to learning from systems established in responding to Ebola?
NERC tried to start a culture change in the way government business is done and accounted for in the name of citizens in Sierra Leone. Lesson-learning was ingrained into NERC’s DNA. Every time a new operation began, indicators were established against which the success of the project could be measured. For example, when a village was quarantined, data would be gathered on how many people were fed and what medical equipment was needed. Close monitoring of our operations was followed by periods of lesson-learning. It did not stop there.
Mechanisms were introduced to take the lessons learned and apply them to future interventions. For example, we had several instances of people who had been exposed to Ebola victims escaping from quarantine and starting new infection hotspots elsewhere. Whilst we improved security, started tracing mobile phone calls and taking other measures to reduce the chances of escape, we also started to ask ourselves why someone facing the risk of a terminal illness would run from us when the whole reason we were isolating them was to be able to help them if they fell ill. The answer lay in the way we were doing the isolation, in recognising our failure to reassure people about their loved ones we had taken into treatment and other logistical issues around their welfare. We changed quarantine protocols and improved the service. Fewer people ran after those changes.
If we could defeat Ebola, why could we not get the basics of running a country – roads, hospitals and schools – right?
To build resilience in a system, you have expose it to problems. For each problem you find, recalibrate that system so that it prevents it from happening again, or highlight it immediately so you can take direct remedial action. At NERC we hunted problems, whereas the norm in Sierra Leone is to try and cover them up. This is because our political economy is set up to feed patronage networks, and not with continuity and transparency in mind. I would like to think that NERC’s successful approach to fighting Ebola has prompted deep introspection within government circles in Sierra Leone. If we could defeat Ebola, why could we not get the basics of running a country – roads, hospitals and schools – right?
At the end, we oversaw a comprehensive review of NERCs operations.9 President Koroma chaired the meeting where the findings were presented and was very keen that this new way of doing business – convergence to excellence, reliance on local structures, decentralisation of power, an open system of accountability and responsibility, a culture of problem-solving and not finger-pointing, and evidence-based policymaking – be adopted into the President’s Recovery Priorities (PRPs).10 So far, there have been some positive initial signs of continuity.
Yvonne Aki-Sawyerr, director of planning at NERC, is now the delivery team lead for implementation of the PRPs. I see this continuity as a conscious and explicit effort by the government to absorb the commitment to evidence-based policymaking and rigorous monitoring and evaluation we championed at NERC. There are very clear timelines put in place for when PRP activities should be complete. People who are accountable for ensuring that happens are known and named; and Sierra Leoneans are informed of what to expect and what role they can play. There are also efforts to ensure greater interaction with, and support for, communities and community-led initiatives, both at the design and implementation stages. The PRP’s creation of chieftaincy engagement officers is one example of an effort to replicate the kind of granular accountability we instilled at NERC.
In October 2016, the country held its first-ever national accountability forum aimed at enforcing improved service delivery. But I am realistic. We did not change the culture with this one initiative, nor can you even say that it has been embedded until two or three similar initiatives emerge and do well. It will be a slow and tortuous process.
ON LEARNING ON THE JOB
How did you approach the many challenges that you faced at NERC? Were there areas where you could have made improvements? And how much freedom did you allow for innovative responses to unique challenges?
The key thing to remember about NERC is that no one was an Ebola expert. We were all learning as we went along – we never had the attitude that we already had the answers. Instead, the approach was to establish a set of guiding principles, to commit to excellence and to embrace the problems we encountered, not run away from them.
One of the first issues I confronted after joining NERC was concern about management of the fleet of vehicles involved in the response: drivers syphoning fuel from tanks or coming to work drunk, and the fact that many of the vehicles had broken down. When I asked for a list of all vehicles that had been bought or donated to the country to fight Ebola, for their fuel forecasts and maintenance schedules, none were forthcoming because they did not exist.
A fleet management system was established to ensure vehicles were properly maintained. Very strict controls were established about who could drive the vehicles, licensing procedures were tightened up, regular spot checks were introduced and a detailed record of each vehicle’s movements was kept, using their unique engine numbers. This system inspired confidence among international donors and gradually they committed funds to ensure that all vehicles being used to tackle Ebola had free maintenance and fuel.
Government cannot force policies down the throats of people, even when it is for their own good
Some strategies could have been better thought through or executed. We could have organised the payment system for health care workers and burial teams better. Even though NERC has been commended for the way it used IT to quickly solve a major problem, it was not as efficient as it could have been. People still went unpaid for far too long. Our social mobilisation messaging could also have been handled better, especially at the start of the outbreak. We could have dealt with quarantine better. It improved towards the end, but for a time it was not as nuanced as it should have been. We did not identify potential contacts outside the home well enough, and failed to provide sufficient welfare supplies on time to those in quarantine. We tried to learn from our mistakes and improve. We did not hide from them.
We had to innovate a great deal. For example, we faced a problem whenever a chief or someone powerful in a traditional secret society died – especially in the rural areas. These societies have ceremonies and rites they perform, but we were insisting on people being buried with full contamination protection and only by our well-protected and trained burial teams. So, to avoid our surveillance, they started burying at night. The women did the same. Our teams started finding fresh graves in villages, with chiefs swearing they knew nothing. The easy option would have been to arrest them for violating the emergency laws on handling corpses we had put in place. Instead, we took our time to understand why they were doing secret burials. Once we found out, we decided to train members of male and female secret societies into burial teams. That way they could follow their traditions and be safe. Reports of secret burials declined significantly. The innovation here was working with the people. Instead of getting carried away with blindly enforcing the rules, we tried to understand why they were breaking them in the first place. Lesson: government cannot force policies down the throats of people, even when it is for their own good.
ON CAPACITY AND LEGACY
Did working on the Ebola response make you more or less optimistic about the future of Sierra Leone?
Working at NERC made me more hopeful for the country. The advent of the virus revealed the worst in some Sierra Leoneans, showing us that there were people who were willing to enrich themselves while their fellow citizens died for lack of resources and to shun others in need. It highlighted our lack of leadership, accountability and social responsibility in some areas. At the same time, it revealed things that I had never before seen in my country. I have never seen people come together in the way they did. I have never seen young people take such control in solving a major problem facing their country. I have never seen the level of convergence to excellence that I saw at NERC, because Ebola did not allow people to take shortcuts.
The fact that predominantly young Sierra Leoneans demonstrated they could work collaboratively to such high standards, and generate their own best practice ideas without everything being handed to them on a plate by some foreign “expert”, gives me a huge amount of hope for the future
When I arrived at the Situation Room, my staff included junior Sierra Leonean civil servants, highly trained and professional Sierra Leonean and British military officers, and staff from the UN and a number of NGOs. The most important of these was the African Governance Initiative, which supported us with several highly capable analysts and advisers at no cost to the government. I partnered up all my Sierra Leonean staff with their more experienced international colleagues and started a training programme in the Situation Room – in the middle of the crisis! This programme developed into the Situation Room Academy.
By the time we closed NERC in January 2016, the Academy had trained – at NERC and in the field – over 1,000 people in data analysis and software tools. We established a Situation Room Mapping Service, which produced maps for everyone – including the UN and British military, who had been making maps for us. We supported a mapping course at Njala University. In the beginning, I had relied on foreign staff to do most of the high-level analysis. By the end, we had only one foreign staff member in the Situation Room. We achieved these things because I was lucky to have a group of highly dedicated and hardworking Sierra Leonean staff who were committed to doing their best, and international colleagues who were committed to passing on their skills as they helped us fight. This was not just at NERC. It happened everywhere in the field. Nurses, doctors, disease surveillance officers, social mobilisers, lab technicians, blood sample collectors and others working with NGOs, learned lessons from their own experiences and demonstrated their ability to match the exacting standards required to fight Ebola.
NOTES
- “2014 Ebola Outbreak in West Africa – Case Counts”, Centers for Disease Control and Prevention, 13 April 2016
- Ross, Emma et al “Sierra Leone’s Response to the Ebola Outbreak: Management Strategies and Key Responder Experiences”, Chatham House, 31 March 2017
- The permanent members were the CEO of NERC (Major (Rtd.) Paolo Conteh); the President’s special adviser on Ebola (Prof. Monty Jones); National Operations Coordinator (Steven Gaojia); Director of Plans (Mahmood Idriss, followed by Yvonne Aki-Sawyerr); Director of Field Operations (Brigadier General DTO Taluva); NERC Situation Room Director (O B Sisay); the Inspector General of Police (Francis Munu – represented by Assistant Inspector General Al Sheik Kamara); the Chief Medical Officer (Dr Brima Kargbo); and any other person the agenda for that meeting dictated as necessary
- US Embassy, British Foreign & Commonwealth Office, DFID, CDC, Chinese Center for Disease Control and Prevention, African Union and others
- For more on the work of the Auditor General in Sierra Leone see “Lara Taylor-Pearce: On transparency and accountability in public financial management”, Africa Research Institute, October 2016
- “Sierra Leone Kerry Town Ebola Treatment Facility”, DFID Development Tracker
- Fitzgerald, Felicity, “Ebola Diary: The junior doctors saving Sierra Leone”, The Daily Telegraph, 23 February 2015
- Government of Sierra Leone, “Government Budget and Statement of Economic Financial Policies”, 11 November 2016
- “Lessons from the Response to the Ebola Virus Disease Outbreak in Sierra Leone, May 2014 to November 2015: Summary Report”, National Ebola Response Centre, 7 November 2015
- The President’s Recovery Priorities is a multi-stakeholder programme of investment, led by the Government of Sierra Leone, which focuses on education, energy, governance, health, private sector development, social protection and water. The programme is intended to drive sustainable socio-economic transformation in Sierra Leone, following the twin shocks of Ebola and falling commodity prices
Omaru Badara (OB) Sisay was Director of the Situation Room at Sierra Leone’s National Emergency Response Centre during the Ebola crisis. He was subsequently awarded a Gold Medal by the President of Sierra Leone and appointed an Officer of the Order of the British Empire (OBE) by HRH Queen Elizabeth II.
Sisay is a strategic intelligence analyst who advises on political, economic, financial and security risk across sub-Saharan Africa.